Introduction
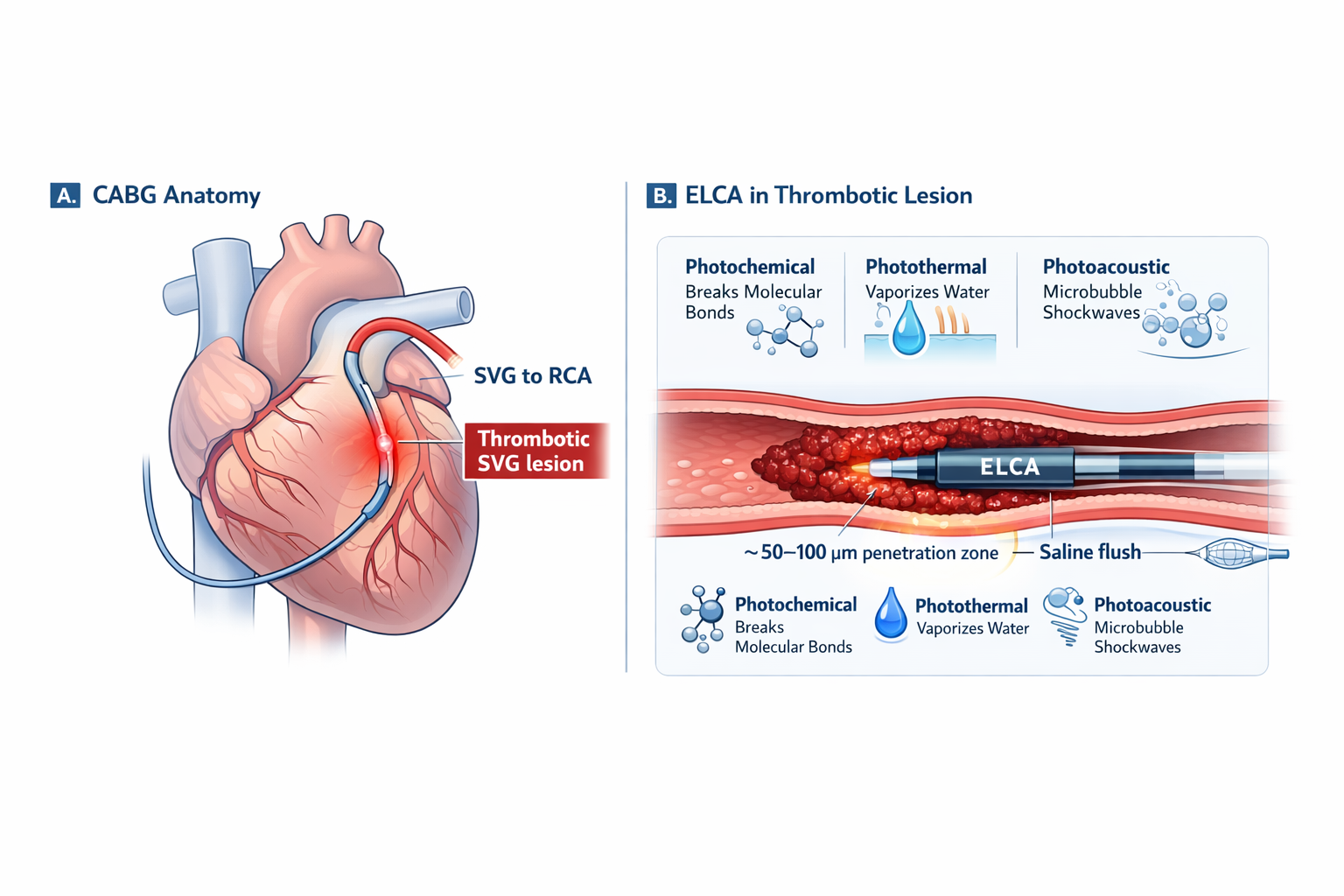
Percutaneous coronary intervention (PCI) in saphenous vein grafts (SVGs) represents one of the most technically demanding areas of contemporary interventional cardiology. SVGs degenerate over time, developing friable atheroma, lipid-rich plaques, and large thrombus burden. These pathological features significantly increase the risk of distal embolization, slow-flow, and no-reflow phenomena—often resulting in poor procedural outcomes and adverse clinical events.
In such high-risk settings, traditional balloon angioplasty or direct stenting may worsen distal embolization rather than improve myocardial perfusion. This is where Excimer Laser Coronary Angioplasty (ELCA) becomes particularly valuable.
ELCA enables controlled thrombus debulking and plaque modification without aggressive mechanical force. When used with proper technique, embolic protection, and intravascular imaging, ELCA can convert an otherwise hazardous SVG intervention into a predictable and safer procedure.
This blog presents a video-guided, real-world ELCA case, structured exactly according to the original slide sequence, clearly guiding which cath-lab video to embed at each stage using the exact video names from the slides.
Understanding ELCA: Why It Works in Thrombotic SVGs
Excimer Laser Coronary Angioplasty uses 308-nm ultraviolet laser energy to ablate thrombus and plaque at a microscopic level. Unlike rotational or orbital atherectomy, ELCA is a non-mechanical modality and works through three synergistic mechanisms:
-
Photochemical effect: Breaks molecular bonds within thrombus and plaque
-
Photothermal effect: Vaporizes intracellular water
-
Photomechanical effect: Generates micro-cavitation bubbles that disrupt lesion architecture
These effects allow ELCA to effectively reduce thrombus burden while minimizing vessel wall trauma—an essential advantage in degenerated SVGs.
Patient Background and Clinical Presentation
The patient was a 77-year-old male with long-standing cardiovascular disease. His medical history included hypertension, type 2 diabetes mellitus, and significant coronary artery disease requiring coronary artery bypass grafting (CABG) in 2001. The bypass strategy included a LIMA to LAD and saphenous vein grafts to the obtuse marginal and posterior descending artery (PDA).
He had undergone PCI to SVGs in 2017 and had a permanent pacemaker implanted in 2019. He presented with chest pain on exertion for one week, with acute worsening over the previous 24 hours.
Clinical evaluation, cardiac biomarkers, and echocardiography were consistent with acute coronary syndrome (NSTEMI) with mild left ventricular dysfunction. Given his graft-dependent circulation, urgent coronary angiography was performed.
Native Coronary Angiography: Establishing the Baseline
Angiography of the native coronary arteries demonstrated chronic occlusions, confirming that the patient’s myocardial perfusion was almost entirely dependent on bypass grafts.
Left System (Native)
Right System (Native)
These videos provide essential anatomical context and explain why intervention on the grafts was critical for myocardial salvage.
Graft Angiography: Ruling Out Non-Culprit Vessels
Subsequent graft angiography revealed that:
-
The SVG to OM was patent
-
The LIMA to LAD demonstrated good flow
There was no evidence of acute thrombotic pathology in these grafts.
SVG to OM
LIMA to LAD
At this point, attention was directed toward the remaining graft supplying the inferior territory.
Culprit Lesion Identification: Thrombotic SVG to PDA
Angiography of the SVG to PDA revealed a large thrombotic occlusion with compromised distal flow. This lesion was clearly identified as the culprit responsible for the patient’s NSTEMI.
SVG to PDA – THROMBOTIC OCCLUSION !
This video is central to the case and should be prominently embedded, as it defines the procedural challenge and rationale for ELCA use.
Procedural Strategy: Why ELCA Was the Preferred Approach
Given the heavy thrombus burden and the fragile nature of degenerated SVG plaque, a conventional balloon-first strategy was considered unsafe. The procedural goals were to:
-
Reduce thrombus burden in a controlled manner
-
Minimize distal embolization
-
Optimize vessel preparation before stenting
An ELCA-assisted PCI strategy, combined with distal embolic protection and intravascular imaging, was therefore planned.
ELCA Technique: First Laser Run
The procedure began with a low-energy ELCA run, performed under continuous saline infusion to prevent laser-contrast interaction. This initial run aimed to gently modify the thrombus without causing distal embolization.
Post 1st Run of ELCA
This video demonstrates the early effect of ELCA and sets the foundation for further energy escalation.
Stepwise Energy Escalation: Second and Third Runs
Following the initial laser pass, ELCA energy was increased in a controlled, stepwise fashion. This gradual escalation is critical for safety and effectiveness.
-
Second run: Fluence 55 mJ/mm², Rate 55 pulses/sec
-
Third run: Fluence 60 mJ/mm², Rate 60 pulses/sec
Second run – Fluence 55 mJ/mm², Rate 55 pulses/sec
Third run – Fluence 60 mJ/mm², Rate 60 pulses/sec
These videos highlight how careful energy escalation can significantly reduce thrombus burden without vessel injury.
Assessing the Impact of ELCA
Following completion of the laser runs, angiography demonstrated improved antegrade flow and a marked reduction in thrombus burden.
Post 3rd ELCA run
This step confirms that the vessel is adequately prepared for definitive PCI.
Preventing Distal Embolization: Embolic Protection Strategy
SVG interventions carry a high risk of distal embolization. To mitigate this risk, a distal embolic protection device was deployed distal to the lesion.
Spider FX™ Embolic Protection Device
This step is essential in SVG PCI and plays a major role in preventing slow-flow and no-reflow phenomena.
Intravascular Imaging: IVUS-Guided Optimization
Intravascular ultrasound (IVUS) was used to assess:
-
Vessel size
-
Residual thrombus
-
Lesion length
-
Optimal stent sizing
IVUS
IVUS guidance ensured accurate stent selection and optimal expansion.
Stent Deployment and Optimization
Following lesion preparation, a drug-eluting stent was deployed across the treated segment.
4.0x16mm Synergy Megatron
To ensure complete lesion coverage and durable results, an additional stent was placed.
4.0x24mm Synergy Megatron
Post-dilatation was performed to achieve optimal stent expansion.
Final Steps and Angiographic Outcome
After completion of PCI, the embolic protection device was carefully retrieved.
Removal of Distal Protection Device’
Final Result
Final angiography demonstrated TIMI 3 flow, excellent distal runoff, and no evidence of distal embolization or procedural complications.
Key Clinical Takeaways
This case highlights several important lessons:
-
ELCA enables controlled thrombus debulking in high-risk SVG lesions
-
Stepwise energy escalation improves procedural safety
-
Distal embolic protection is critical in SVG PCI
-
IVUS guidance optimizes stent selection and expansion
This video-guided case clearly demonstrates how Excimer Laser Coronary Angioplasty, when used thoughtfully and systematically, can transform the management of complex thrombotic SVG lesions. By combining ELCA with embolic protection and intravascular imaging, interventional cardiologists can achieve excellent angiographic and clinical outcomes even in the most challenging scenarios.
For operators dealing with degenerated graft disease, ELCA remains an indispensable tool in the modern PCI armamentarium.
About the Doctor
DR. V. RAJASEKHAR
MD, DM (Cardiology)
CARDIOLOGY | 27 YRS
Yashoda Hospitals, Hitech City, Hyderabad