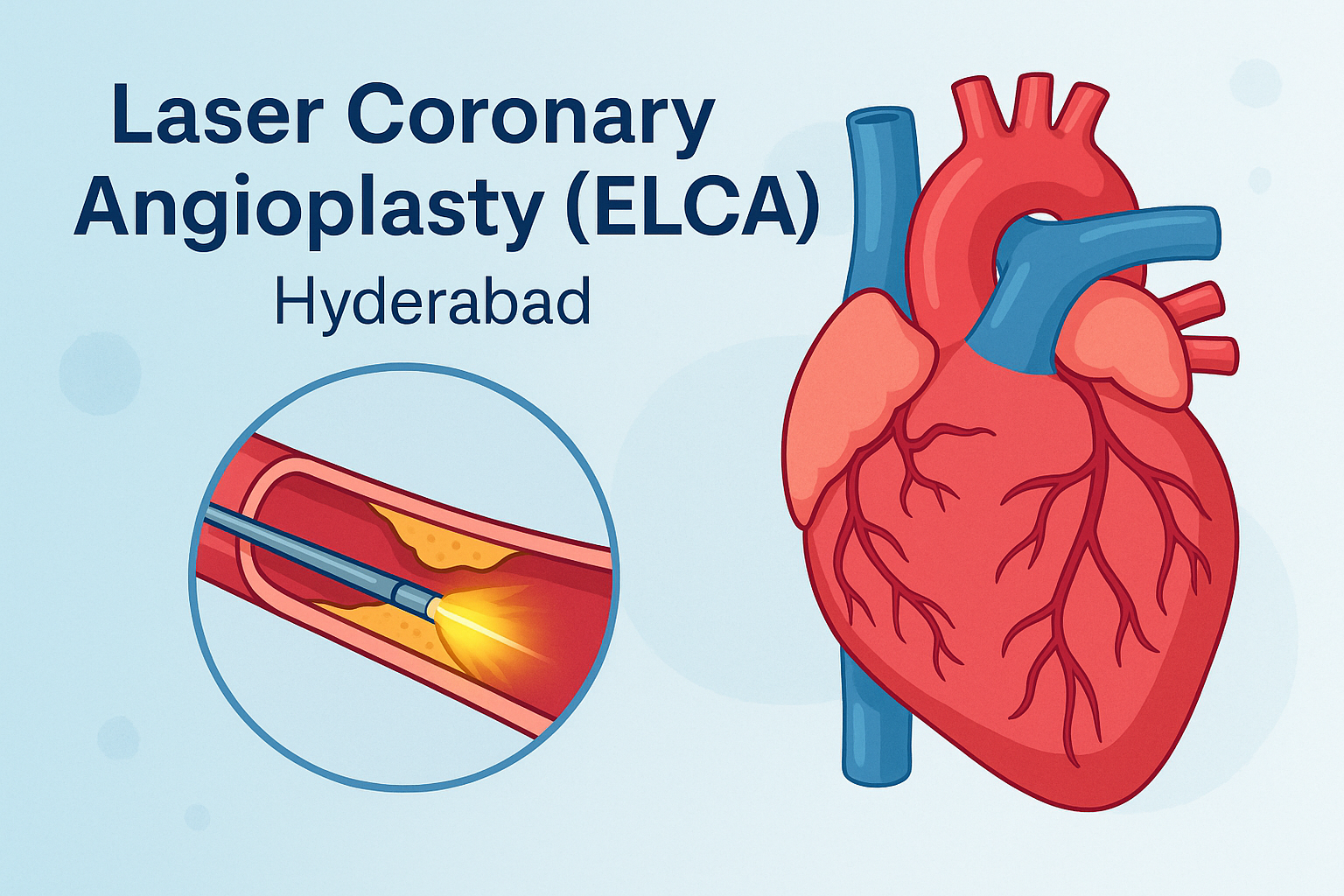
Thinking about laser coronary angioplasty in Hyderabad? Learn how ELCA works, who needs it, benefits vs. other calcium-modification options, risks, recovery, and FAQs—written for patients and families.
TL;DR (30-second summary)
-
Laser Coronary Angioplasty (ELCA) uses ultraviolet (308 nm) laser energy delivered via a tiny catheter to vaporize and modify plaque or thrombus inside narrowed heart arteries. It’s especially helpful when balloons won’t cross/open, in-stent restenosis (ISR), under-expanded stents, thrombus-rich lesions, and certain chronic total occlusions (CTO).
-
In Hyderabad—from Banjara Hills, Jubilee Hills, Somajiguda, HITEC City, Gachibowli, and Secunderabad—tertiary cardiac centres increasingly pair ELCA with intravascular imaging (IVUS/OCT) to plan and confirm results, often followed by ballooning/stenting.
-
ELCA is not a replacement for stents; it’s a lesion-preparation tool that can improve stent expansion and outcomes when used in the right patients.
Medical disclaimer: This guide is educational and not a substitute for clinical advice. Decisions must be made with your interventional cardiologist.
What is Laser Coronary Angioplasty (ELCA)?
ELCA stands for Excimer Laser Coronary Atherectomy. During a minimally invasive heart procedure (PCI), a cardiologist advances a soft guidewire into the diseased artery, tracks an ELCA catheter over it, and delivers pulsed UV laser to photo-ablate (vaporize) obstructive material. Unlike mechanical rotors or burrs, ELCA has no rotating metal parts; the tissue effect is created by light.
The 3 ways ELCA works inside the artery
-
Photochemical: UV photons break molecular bonds in plaque material.
-
Photothermal: Rapid heating of intracellular water causes micro-rupture of cells.
-
Photomechanical: Tiny vapor bubbles expand/implode, mechanically disrupting debris.
Wavelength: The laser is typically 308 nm (xenon-chloride excimer)—well absorbed by tissue and water—delivered in very short pulses.
When do doctors consider ELCA?
ELCA is not used in every angioplasty. It is particularly considered when a standard balloon or stent strategy is difficult or unsafe without prior “lesion modification.” Common scenarios include:
-
Balloon-uncrossable or undilatable lesions (hard plaque that balloons can’t open)
-
In-stent restenosis (ISR) and under-expanded stents
-
Thrombus-rich lesions (e.g., some acute coronary syndromes)
-
Ostial, long (>20 mm), or moderately calcified lesions
-
Saphenous vein graft lesions
-
Select CTOs after guidewire passage
During lasing, cardiologists often infuse saline through the guide catheter to minimize bubbles and reduce the risk of dissections—this technique enhances safety.
Step-by-step: How ELCA is performed (Hyderabad care pathway)
-
Evaluation & planning: History, exam, ECG, echocardiography, kidney function tests, and coronary angiography. IVUS/OCT may be planned to measure plaque burden and calcium.
-
Access & wiring: Through a small wrist (radial) or groin (femoral) artery, a guide catheter hooks the coronary ostium; a 0.014″ guidewire crosses the lesion.
-
Laser catheter delivery: An ELCA catheter is advanced to the lesion. The operator sets fluence (energy) and repetition rate, then delivers short laser runs, typically while saline is infused.
-
Check and optimize: Re-imaging (angiography ± IVUS/OCT) gauges debulking; adjunctive balloon angioplasty, specialty balloons, IVL, or stenting may follow to achieve an optimal result.
-
Hemostasis & recovery: Post-procedure monitoring (often overnight), antiplatelet therapy per guideline-directed care.
Benefits of ELCA
-
Versatility in complex anatomy: Can treat mixed morphologies, ISR, thrombus, and some calcified lesions—useful when other devices can’t cross or open.
-
No rotating hardware: Reduces risk of entanglement with stent struts compared with mechanical devices in selected ISR/under-expanded stents. (Device choice remains patient-specific.)
-
Synergy with imaging: When paired with IVUS/OCT, ELCA can help achieve better stent expansion—an established driver of long-term outcomes.
ELCA vs. other calcium-modification tools
Rotational/OA (burrs/crowns) mechanically sand calcium; IVL (intravascular lithotripsy) cracks calcium with acoustic waves; ELCA photo-ablates plaque/thrombus and modifies tissue by UV energy.
-
Contemporary reviews show comparable procedural success between laser and rotational atherectomy in selected lesions; the choice is individualized based on lesion type, operator experience, and imaging findings.
-
In under-expanded stents or ISR with fibro-calcific tissue, operators may prefer ELCA (sometimes combined with contrast-assisted techniques in specialized centers) or IVL, guided by IVUS/OCT.
Who is a good candidate in Hyderabad?
Your interventional cardiologist may discuss ELCA if you have recurrent angina, positive stress tests, or coronary angiography showing ISR, heavily modified lesions that balloons can’t open, or thrombus-laden blockages. Multi-disciplinary, patient-centered decision-making aligned with ACC/AHA/SCAI PCI guidelines is standard.
Risks & safety
All coronary interventions carry risk. With ELCA, potential complications include coronary dissection or perforation, spasm, slow/no-reflow, arrhythmias, and contrast-related kidney issues. ELCA should be performed in hospitals capable of immediate emergency bypass surgery in rare catastrophic events; this is part of device labeling and IFU cautions.
Regulatory note: ELCA catheters (Spectranetics/Philips) are FDA-approved and used with the Philips Laser System (PLS/CVX-300).
Recovery & follow-up
Most Hyderabad patients go home the next day after an uncomplicated PCI. You’ll receive instructions on activity, wound care, medicine adherence (usually dual antiplatelets if stented), and a timeline for return to work and cardiac rehab. Follow-ups may include lipid goals, blood pressure/sugar control, and lifestyle changes (diet, exercise, smoking cessation).
Costs & insurance (Hyderabad)
Costs vary by hospital tier, device use, number of stents, imaging (IVUS/OCT), and length of stay. In India, ELCA is a specialized add-on tool, so procedures that use it may be priced higher than standard angioplasty. Confirm coverage with your insurer/TPA and the cath-lab coordinator for an accurate estimate tailored to your case.
Why Hyderabad?
Hyderabad’s high-volume cardiac centres offer 24×7 primary PCI, intravascular imaging, and a full toolbox (ELCA, rotational/orbital atherectomy, IVL) so operators can match the device to the lesion—a key determinant of safety and long-term success. Shared decision-making that respects your preferences is emphasized in modern PCI care.
Frequently Asked Questions (FAQs)
1) What exactly is laser coronary angioplasty?
It’s a minimally invasive PCI technique that uses a pulsed 308 nm excimer laser to photo-ablate obstructive material (plaque/thrombus) inside coronary arteries, often as a preparation step before balloons and stents.
2) Is ELCA better than standard angioplasty?
“Better” depends on your lesion. ELCA is added when balloons alone won’t cross/open, in ISR/under-expanded stents, or thrombus-rich lesions. Often, ELCA enables ballooning/stenting to be done safely and effectively.
3) Will I still need a stent after ELCA?
Often yes. ELCA prepares the blockage; balloons/stents commonly complete the job. The plan is individualized with imaging guidance.
4) How long does the procedure take?
Similar to complex PCI timings. The laser portion is usually brief, performed in multiple short runs, but overall time depends on lesion complexity and adjunctive steps.
5) Is the laser safe inside arteries?
When used by trained operators following IFU and guidelines, ELCA has acceptable safety for the right indications. Hospitals must be equipped for rare emergencies.
6) Will I feel the laser?
No. You may feel pressure at the access site or chest sensations typical of PCI, but not the laser itself; you’ll be sedated and monitored.
7) How does ELCA compare to rotational atherectomy or IVL?
They’re different tools. Reviews show comparable success in selected cases; choice depends on plaque type (calcium vs. fibrous vs. thrombus), stent issues, and imaging. Many centres in Hyderabad keep all three available.
8) Can ELCA be used for clots during a heart attack?
In selected thrombus-rich lesions, ELCA can help debulk thrombus and facilitate stenting, but decisions are case-by-case.
9) What are the main risks?
Dissection, perforation, spasm, slow/no-reflow, arrhythmia, contrast-related kidney injury, bleeding at the access site—your team will discuss personalized risks and mitigations.
10) How soon can I go home and resume work?
Many patients are discharged within 24 hours after uncomplicated procedures. Return-to-work timing depends on your clinical stability and job type; your cardiologist will advise.
11) Do diabetes, kidney disease, or age prevent ELCA?
Not automatically. Comorbidities increase risk and influence planning (hydration, dye minimization, imaging, access). Your case is individualized under guideline-directed care.
Availability is concentrated in tertiary centres with advanced cath-lab capabilities; ask specifically whether ELCA, IVUS/OCT, and multiple modification tools are on site.